**In the dynamic and often intense environment of labor and delivery, ensuring the well-being of both mother and baby is paramount. At the heart of this critical mission lies vigilant fetal monitoring, a practice that allows healthcare professionals to continuously assess the baby's response to labor. A cornerstone tool for nurses in this endeavor is the "veal chop nursing" mnemonic, a powerful and indispensable guide for interpreting fetal heart rate patterns and implementing timely interventions.** This article delves deep into the significance of veal chop nursing, exploring its components, practical application, and why it remains an essential skill for every labor and delivery nurse committed to optimal maternal and fetal health outcomes. Understanding fetal heart rate patterns is not merely an academic exercise; it's a life-saving skill. The ability to quickly and accurately interpret these patterns, identify potential distress, and initiate appropriate interventions can significantly impact the health trajectory of a newborn. For nurses, the veal chop mnemonic provides a structured, memorable framework that transforms complex physiological data into actionable insights, empowering them to make informed decisions under pressure.
Table of Contents
- What is Veal Chop Nursing? A Critical Mnemonic for Labor & Delivery
- The VEAL CHOP Mnemonic Decoded: Understanding Fetal Heart Rate Patterns and Their Causes
- Why Veal Chop Nursing Matters: Ensuring Optimal Outcomes
- Fetal Heart Rate Monitoring Methods and Goals
- Nursing Responsibilities in Fetal Monitoring
- Timely Interventions: A Nurse's Critical Role
- Continuous Learning and Expertise in Labor & Delivery
- Real-World Application: Case Studies & Scenarios
What is Veal Chop Nursing? A Critical Mnemonic for Labor & Delivery
At its core, **veal chop nursing** refers to the use of a specific mnemonic device by healthcare professionals, primarily labor and delivery nurses, to quickly interpret fetal heart rate (FHR) patterns observed during labor. This mnemonic is a powerful educational tool that helps nurses remember the different types of fetal heart rate changes and, crucially, their underlying causes. As stated in our source data, "Veal chop is a medical and nursing mnemonic used to remember fetal heart rate patterns and their causes." It provides a systematic approach to assessing fetal well-being, enabling nurses to identify whether a pattern is reassuring, non-reassuring, or requires immediate intervention. The importance of this mnemonic cannot be overstated. In the fast-paced environment of a delivery room, rapid assessment and decision-making are vital. The **veal chop nursing** framework simplifies complex physiological responses into an easily recallable format, ensuring that nurses can quickly link an observed fetal heart rate pattern to its most probable cause. This immediate recognition is the first step towards implementing timely and appropriate interventions, which are often critical for optimal maternal and fetal health outcomes. It empowers nurses to "identify and manage variations in fetal heart rate patterns," as highlighted in the provided information.The VEAL CHOP Mnemonic Decoded: Understanding Fetal Heart Rate Patterns and Their Causes
The **veal chop nursing** mnemonic is ingeniously structured, pairing each letter from "VEAL" (representing fetal heart rate patterns) with a corresponding letter from "CHOP" (representing the most common causes). This direct correlation is what makes the mnemonic so effective for rapid recall and application. Let's break down each component:V: Variable Decelerations and C: Cord Compression
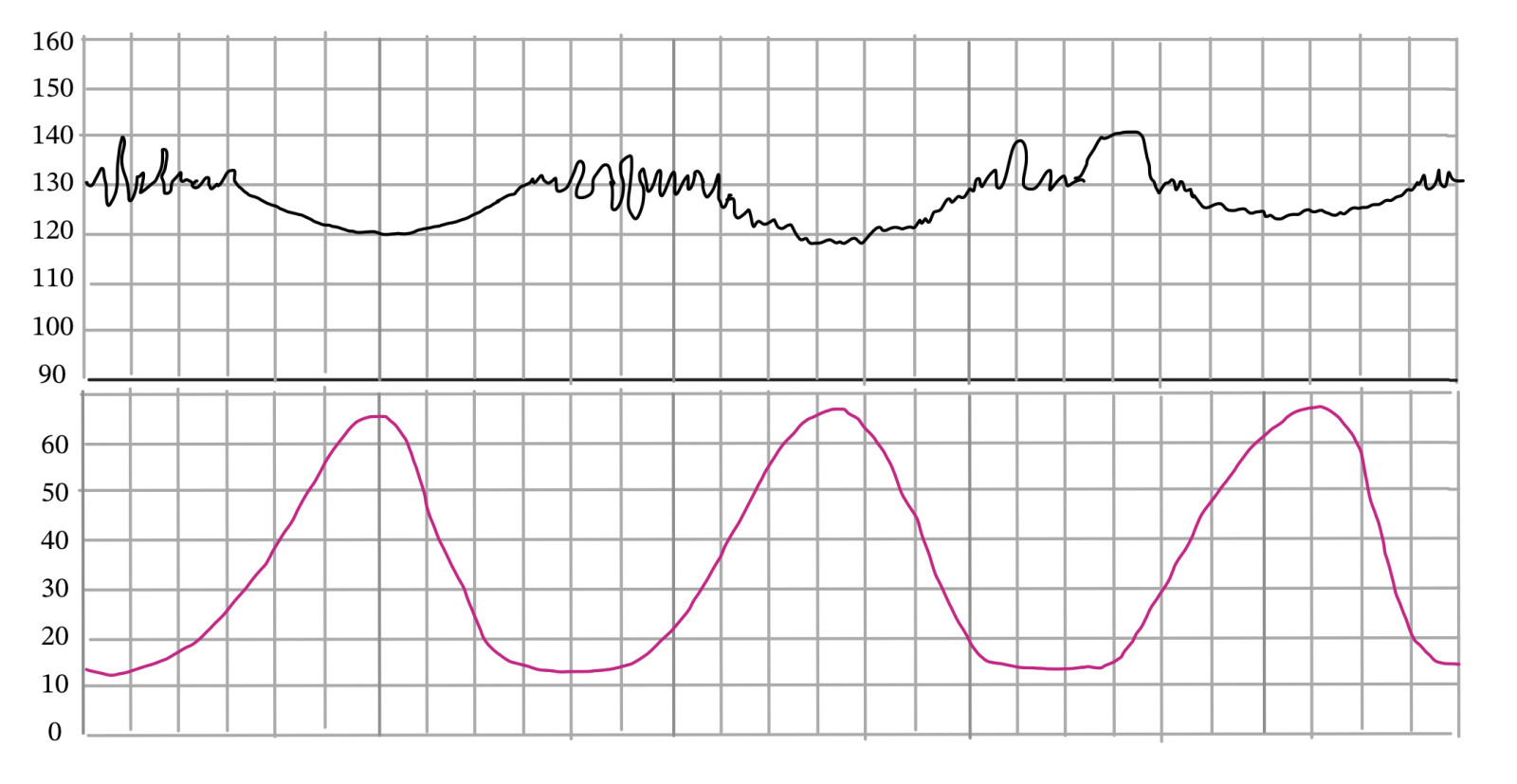
**V stands for Variable Decelerations.** These are abrupt, visually apparent decreases in the fetal heart rate, which can vary in their timing, depth, and duration relative to uterine contractions. They often have a "W" or "U" shape on the fetal heart rate tracing. **C stands for Cord Compression.** This is the primary cause of variable decelerations. When the umbilical cord is compressed, blood flow to the baby is temporarily reduced, leading to a transient decrease in oxygen supply and a reflex slowing of the heart rate. This compression can occur due to various reasons, such as the cord being wrapped around the baby's neck or body, a knot in the cord, or the baby lying on the cord. **Interventions for Variable Decelerations:** The interventions for variable decelerations often focus on relieving the cord compression. These include:- **Maternal Repositioning:** Changing the mother's position (e.g., left lateral, right lateral, hands and knees) can often relieve pressure on the umbilical cord.
- **Amnioinfusion:** If the cause is thought to be oligohydramnios (low amniotic fluid) leading to cord compression, a sterile saline solution can be infused into the uterus to cushion the cord.
- **Oxygen Administration:** Providing supplemental oxygen to the mother may improve oxygenation to the fetus.
- **Discontinuing Oxytocin:** If oxytocin is being administered to augment labor, it may be temporarily stopped to reduce the frequency and intensity of contractions, which can worsen cord compression.
- **Vaginal Examination:** To rule out cord prolapse, which is a medical emergency.
E: Early Decelerations and H: Head Compression
**E stands for Early Decelerations.** These are gradual, symmetrical decreases in the fetal heart rate that mirror the uterine contractions, meaning they begin and end with the contraction. They are typically shallow and return to baseline by the end of the contraction. **H stands for Head Compression.** This is the cause of early decelerations. As the baby's head descends into the birth canal and is compressed by the cervix or pelvic bones during a contraction, it stimulates the vagus nerve, leading to a temporary slowing of the heart rate. Early decelerations are generally considered benign and a sign of fetal well-being and progress in labor. Our source data notes, "Earlys are okay and no." **Interventions for Early Decelerations:** Typically, no specific interventions are required for early decelerations as they are physiological and indicate labor progress. The nurse's role here is primarily to monitor and document the pattern, ensuring it remains consistent with early decelerations and does not progress to other, more concerning patterns.A: Accelerations and O: Okay (or Oxygenated)
**A stands for Accelerations.** These are abrupt, transient increases in the fetal heart rate above the baseline, typically by at least 15 beats per minute (bpm) lasting for at least 15 seconds. In preterm fetuses (less than 32 weeks gestation), an acceleration is defined as an increase of 10 bpm lasting 10 seconds. **O stands for Okay (or Oxygenated).** Accelerations are a reassuring sign of fetal well-being and indicate a healthy, well-oxygenated fetus with an intact neurological system. They demonstrate the fetus's ability to respond to stimuli and are a positive indicator during labor. **Interventions for Accelerations:** No interventions are needed for accelerations. The presence of accelerations is a positive sign and confirms fetal well-being. The nurse's role is to continue monitoring and document this reassuring pattern.L: Late Decelerations and P: Placental Insufficiency
**L stands for Late Decelerations.** These are gradual, symmetrical decreases in the fetal heart rate that begin *after* the peak of the contraction and return to baseline *after* the contraction has ended. They are often shallow but can be profound. **P stands for Placental Insufficiency.** This is the most concerning cause of late decelerations. It indicates that the placenta is not adequately supplying oxygen and nutrients to the fetus, particularly during uterine contractions when blood flow to the placenta is temporarily reduced. This can be due to various factors such as maternal hypotension, preeclampsia, placental abruption, post-term pregnancy, or maternal diabetes. **Interventions for Late Decelerations:** Late decelerations are non-reassuring and require immediate and aggressive intervention to improve fetal oxygenation. These interventions include:- **Maternal Repositioning:** Changing the mother's position (e.g., left lateral) to improve uterine blood flow.
- **Oxygen Administration:** Administering supplemental oxygen to the mother via a non-rebreather mask to increase fetal oxygen supply.
- **Increasing IV Fluids:** Bolusing intravenous fluids to improve maternal hydration and placental perfusion.
- **Discontinuing Oxytocin:** Immediately stopping any oxytocin infusion to reduce uterine activity and allow for better placental perfusion.
- **Notify Healthcare Provider:** Promptly informing the physician or midwife about the non-reassuring pattern.
- **Prepare for Delivery:** Depending on the severity and persistence of the late decelerations, preparations for an expedited delivery (e.g., C-section) may be necessary.
Why Veal Chop Nursing Matters: Ensuring Optimal Outcomes
The importance of **veal chop nursing** extends far beyond simply memorizing an acronym. It is a cornerstone of safe labor and delivery practice, directly contributing to positive maternal and fetal health outcomes. In the context of E-E-A-T (Expertise, Experience, Authoritativeness, Trustworthiness) and YMYL (Your Money or Your Life) principles, the application of veal chop nursing by skilled professionals exemplifies high-quality healthcare. Nurses who master this mnemonic demonstrate expertise in fetal assessment. Their experience in applying it in various clinical scenarios builds their authority in managing labor. The consistent and accurate use of **veal chop nursing** fosters trustworthiness among patients and the wider healthcare team, knowing that fetal well-being is being meticulously monitored. This directly impacts YMYL areas, as decisions made based on fetal heart rate patterns can literally mean the difference between life and death or long-term health complications for a newborn. Discovering "the importance of veal chop nursing, fetal heart rate monitoring, and timely interventions for optimal maternal and fetal health outcomes" is crucial for all involved in childbirth. The mnemonic provides a standardized language for communication among healthcare providers, ensuring that everyone understands the assessment and planned interventions. This clarity is vital in high-stress situations where every second counts.Fetal Heart Rate Monitoring Methods and Goals
Fetal heart rate monitoring is a fundamental aspect of labor and delivery care. It can be performed intermittently or continuously, depending on the mother's risk factors and the stage of labor. As our source data mentions, "Fetal heart rate can be monitored through auscultation by a healthcare" professional, which refers to intermittent monitoring using a Doppler or fetoscope. Continuous electronic fetal monitoring, however, provides a continuous tracing of the fetal heart rate and uterine contractions, which is then interpreted using tools like the **veal chop nursing** mnemonic. The primary goals of fetal heart rate monitoring are:- To assess the fetal oxygenation status.
- To identify signs of fetal distress early.
- To guide interventions that can improve fetal well-being.
- To determine the appropriate timing and method of delivery if fetal compromise is detected.
Nursing Responsibilities in Fetal Monitoring
The role of the labor and delivery nurse in fetal monitoring is multifaceted and extends beyond simply interpreting the tracing. Their responsibilities include:- **Applying and Maintaining Monitoring Equipment:** Ensuring proper placement and functioning of external (tocodynamometer and ultrasound transducer) or internal (fetal scalp electrode and intrauterine pressure catheter) monitors.
- **Baseline Assessment:** Establishing the fetal heart rate baseline and assessing variability.
- **Pattern Recognition:** Accurately identifying and categorizing fetal heart rate patterns (accelerations, early, variable, and late decelerations) using the **veal chop nursing** mnemonic.
- **Documentation:** Meticulously documenting all fetal heart rate patterns, maternal interventions, and fetal responses. This documentation is crucial for legal purposes and continuity of care.
- **Communication:** Effectively communicating findings to the healthcare provider and the patient.
- **Patient Education:** Explaining the monitoring process and findings to the patient and their support person in an understandable manner.
- **Advocacy:** Advocating for the fetus by initiating timely interventions and escalating concerns when necessary.
- **Continuous Assessment:** Recognizing that fetal heart rate patterns can change rapidly and requiring ongoing vigilance.
Timely Interventions: A Nurse's Critical Role
The true power of **veal chop nursing** lies in its direct link to actionable interventions. Once a non-reassuring pattern (like variable or late decelerations) is identified, the nurse's immediate response can significantly alter the outcome. The mnemonic not only helps identify the problem but also guides the nurse towards the most appropriate first-line interventions. For instance, upon recognizing late decelerations (L for Late, P for Placental Insufficiency), a nurse immediately knows to reposition the mother, administer oxygen, increase IV fluids, and discontinue oxytocin. These steps are often referred to as "intrauterine resuscitation" and are designed to improve oxygen delivery to the fetus. The speed and efficacy with which these interventions are implemented are paramount. Delays can lead to worsening fetal acidosis, neurological damage, or even fetal demise. This highlights the "timely interventions for optimal maternal and fetal health outcomes" emphasized in the provided data. Nurses are trained to be proactive, anticipating potential issues and acting decisively.Continuous Learning and Expertise in Labor & Delivery
The field of labor and delivery nursing demands continuous learning and the cultivation of deep expertise. While the **veal chop nursing** mnemonic provides a strong foundation, true mastery comes from extensive experience, ongoing education, and critical thinking. Nurses must not only remember the mnemonic but also understand the underlying physiology, the nuances of different clinical scenarios, and the potential impact of various maternal conditions on fetal well-being. Hospitals, especially those renowned for their maternal-child care, invest heavily in training and education for their labor and delivery staff. For example, a "magnet facility and ranked as #1 children's hospital in the US by US News" would undoubtedly emphasize advanced fetal monitoring education, ensuring their nurses are at the forefront of best practices. Nurses often participate in advanced fetal monitoring courses, simulations, and regular competency assessments to hone their skills. This commitment to professional development ensures that nurses can effectively "interpret fetal heart rate patterns and intervene in labor," continuously refining their ability to provide the highest standard of care.Real-World Application: Case Studies & Scenarios
In practice, **veal chop nursing** is not a static concept but a dynamic tool applied in real-time, often under immense pressure. Consider a scenario where a nurse observes recurrent variable decelerations on the fetal monitor. Immediately, the "V" in VEAL triggers "C" for Cord Compression. The nurse's first action would be to reposition the mother. If the pattern persists, further interventions like amnioinfusion might be considered in consultation with the physician. Another scenario might involve a sudden onset of late decelerations. The nurse, recognizing "L" for Late and "P" for Placental Insufficiency, would swiftly initiate intrauterine resuscitation measures while simultaneously alerting the healthcare provider. These rapid, informed responses, guided by the **veal chop nursing** mnemonic, are what make the difference in critical moments, safeguarding the health of both mother and baby. The ability to apply this knowledge effectively in diverse and unpredictable labor scenarios is a testament to the nurse's expertise and the mnemonic's practical value.Conclusion
The **veal chop nursing** mnemonic is far more than just a memory aid; it is a vital instrument in the arsenal of every labor and delivery nurse. It provides a clear, concise, and actionable framework for interpreting complex fetal heart rate patterns, understanding their causes, and implementing timely, life-saving interventions. By mastering this mnemonic, nurses uphold the highest standards of care, ensuring optimal maternal and fetal health outcomes and embodying the principles of expertise, authority, and trustworthiness that are crucial in healthcare. We hope this comprehensive guide has illuminated the profound importance of **veal chop nursing** in the intricate world of labor and delivery. Your insights and experiences are invaluable. Have you encountered a situation where the veal chop mnemonic proved critical? Share your thoughts and experiences in the comments below, or consider sharing this article with fellow healthcare professionals to spread awareness about this indispensable tool. For more in-depth articles on maternal and child health, explore our other resources on this site.Related Resources:
Detail Author:
- Name : Davonte Barrows
- Username : baylee52
- Email : jailyn39@cole.com
- Birthdate : 1998-04-11
- Address : 104 Tillman Ford Suite 155 Kristamouth, KY 55659
- Phone : 956-232-4349
- Company : Zemlak, Erdman and McDermott
- Job : Chemistry Teacher
- Bio : Eius sapiente omnis sed. Dolorem ipsum eum aut quae. Excepturi ducimus fugiat amet.
Socials
linkedin:
- url : https://linkedin.com/in/jankunding
- username : jankunding
- bio : Quisquam aliquam velit ratione.
- followers : 6975
- following : 1403
facebook:
- url : https://facebook.com/julia1022
- username : julia1022
- bio : Rem repudiandae molestias expedita ipsa totam.
- followers : 2503
- following : 1708